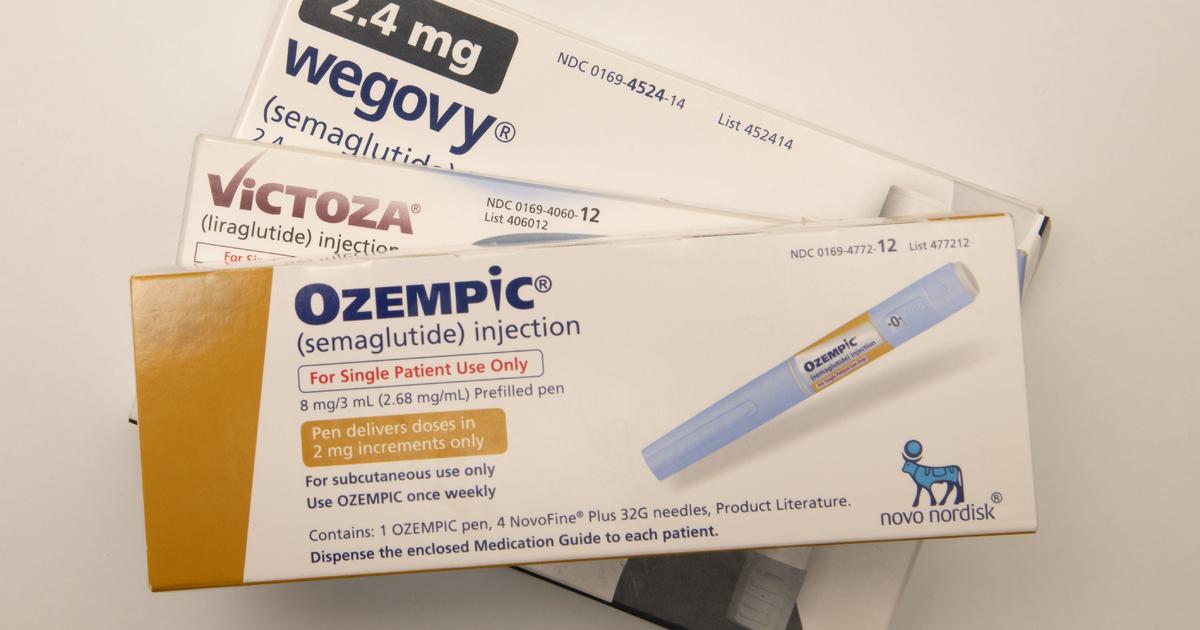
Drugs like Wegovy, Ozempic would be covered by Medicare, Medicaid under Biden proposal
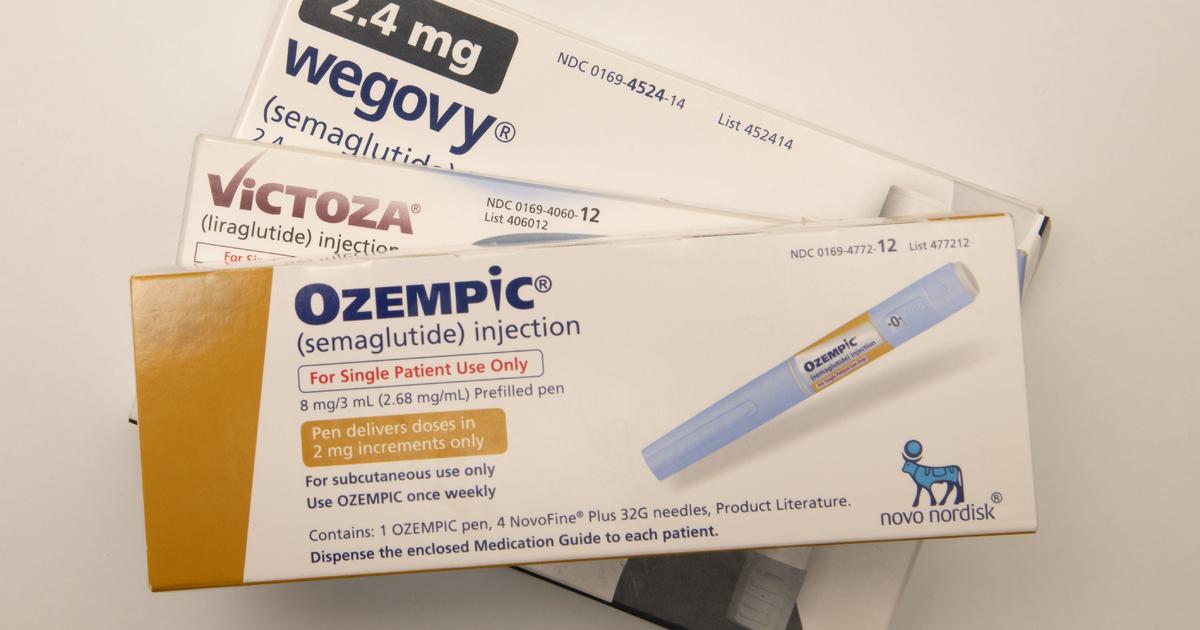
Washington — Millions of Americans with obesity would be eligible to have popular weight-loss drugs like Wegovy or Ozempic covered by Medicare and Medicaid under a new rule the Biden administration proposed Tuesday morning.
The costly proposal from the U.S. Department of Health and Human Services sets the stage for a potential showdown between the powerful pharmaceutical industry and Robert F. Kennedy Jr., an outspoken opponent of the weight-loss drugs who, as President-elect Donald Trump’s nominee to lead the department, could try to block the measure.
While the rule would give millions of people access to weekly injectables that have helped people shed pounds so quickly that some have labeled them miracle drugs, it would cost taxpayers as much as $35 billion over the next decade.
proposal, Medicare and Medicaid coverage would extended to people prescribed the drugs “to reduce excess body weight and maintain weight reduction long-term for individuals with obesity.”
Medicare estimates most obese enrollees are already eligible through other conditions, like diabetes, heart disease or sleep apnea. Around 7% of Medicare beneficiaries would be newly eligible.This means people who are only overweight but not obese would still not be covered, unless it was paired with another qualifying condition like treating diabetes or heart disease.
The change also applies to state Medicaid programs, which would now no longer be allowed to exclude coverage of weight loss drugs for obese residents.
The Centers for Medicare and Medicaid Services estimates that 12% of adults covered by Medicaid would be newly eligible. Adolescents could also be covered, given the Food and Drug Administration has approved use of Wegovy down to age 12.
The anti-obesity drug market has expanded significantly in recent years, with the FDA approving a new class of weekly injectables like Novo Nordisk’s Wegovy and Eli Lilly’s Zepbound to treat obesity.
People can lose as much as 15% to 25% of their body weight on the drugs, which imitate the hormones that regulate appetites by communicating fullness between the gut and brain when people eat.
The cost of the drugs has largely limited them to the wealthy, including celebrities who boast of their benefits. A monthly supply of Wegovy rings up at $1,300 and Zepbound will put you out $1,000. Shortages of the drugs have also limited the supplies.
When would coverage of weight loss drugs start?
For Medicare, the proposal to require Part D plans to expand coverage for weight loss drugs would take effect for plans in 2026.Officials claimed they do not think the proposal will lead to significantly increased costs for seniors next year, citing provisions in the Inflation Reduction Act.
“We do not expect any short-term impact on premiums from this proposal, and in fact, this proposal provides a significant savings for people who currently may be paying out of pocket for these medications,” Dr. Meena Seshamani, the top official overseeing Medicare, told reporters.
It is unclear when the proposal would take effect in state Medicaid programs.
Centers for Medicare and Medicaid officials said they are inviting public comment on when states should be required to cover the costly medications.”States are also feeling substantial state budget pressure and we are doing our part to make sure patients, Medicaid enrollees all across the country can get access,” Dan Tsai, the agency’s top Medicaid official, told reporters.
Over the next decade, the proposal would cost the federal government $11 billion and states $3.8 billion, they estimated.”We would urge drug manufacturers to do their part as well, make sure they’re thinking about offering fair, appropriate prices to the Medicaid program,” Tsai said.
The path forward in new administration is unclear
While it’s unclear where Trump himself stands on coverage of the weight-loss drugs, his allies and Cabinet picks who have vowed to cut government spending could balk at the upfront price tag
Medicare has been barred from offering the drugs under a decades-old law that prohibits the government-backed insurance program from covering weight-loss products. The rule proposed by the Biden administration, however, would recognize obesity as a disease that can be treated with the help of the drugs.
Kennedy, who as Trump’s nominee for HHS secretary is subject to Senate confirmation, has railed against the drugs’ popularity. In speeches and on social media, he’s said the U.S. shouldn’t cover the drugs through Medicaid or Medicare. Instead, he supports a broad expansion of coverage for healthier foods and gym memberships.
“For half the price of Ozempic, we could purchase regeneratively raised, organic food for every American, three meals a day and a gym membership, for every obese American,” Kennedy said to a group of federal lawmakers during a roundtable earlier this year.
Alexander Tin
contributed to this report.
Source: cbsnews.com